VELTRIX HEALTH MEDICAL REVENUE CYCLE MANAGEMENT SERVICE
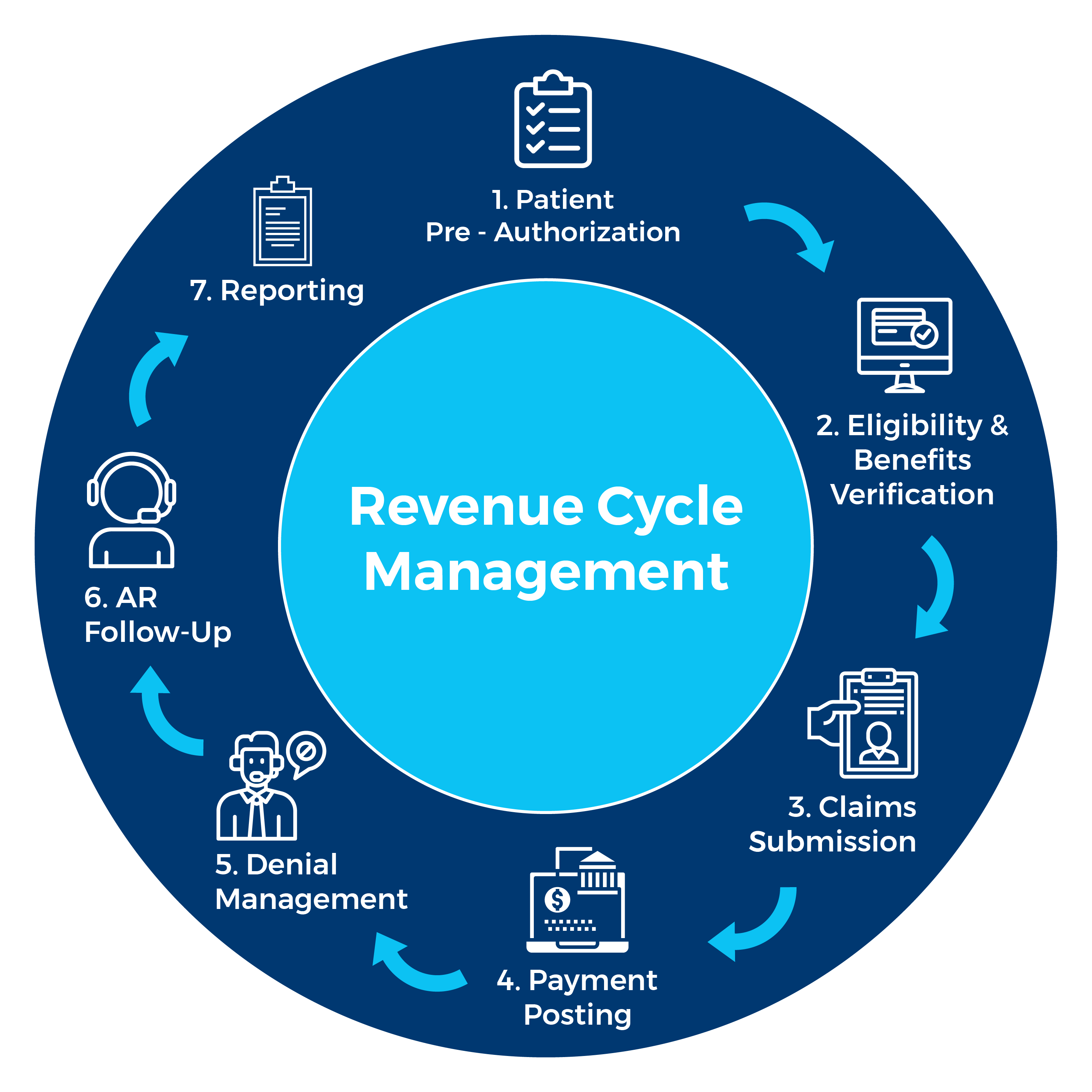
Veltrix Health's Medical Revenue Service generates and collects payments for healthcare providers' services. It covers all revenue cycle management aspects, including patient registration, insurance verification, coding, billing, and collections. By optimizing the revenue cycle, our RCM solution helps improve the financial performance of the physician's medical center.
Get a Complementary Analysis
Importance of Choosing Urgent RCM Revenue Cycle Management Service in Medical Billing
Managing the finances of a medical practice is complicated. With ever-changing regulations, strict insurance policies, and patients with high expectations, it can lead to revenue loss, cash flow issues, and operational problems.
Remember this: Veltrix Health's medical revenue cycle management (RCM) experts can help your practice improve its finances. Our certified coders ensure billing and coding are accurate to prevent revenue loss. Our enrollment specialists secure contracts with major commercial payers to expand your patient base. Our billing experts work hard to collect all the money your practice earns.
Don't let medical expenses stress you out. Veltrix Health Medical Revenue Service can help improve your practice's finances. Contact us today to see how we can optimize your revenue cycle process to increase collections and improve patient satisfaction.

Achieve revenue cycle success via Veltrix Health coding excellence
Veltrix Health medical revenue service improves revenue cycles through expert medical coding. Our BellCoding technology reviews medical charts to find high-value codes. Our coders, with CPC certifications, review each chart to find revenue opportunities that algorithms miss. Combining human expertise with technology, Veltrix Health provides an RCM solution that helps healthcare facilities increase their revenue.
Contact Us
Veltrix Health offers revenue cycle care, with billing at its core
Our RCM Service's method of handling medical billing leads to clear improvements in the revenue cycle process. Our in-house system examines billing codes and clinical documentation to identify issues before submitting claims. This technology results in first-time acceptance rates of over 98%, allowing our providers to receive payment more quickly.
Contact UsUp To 30% Revenue Increase In Next 12 Months With
Veltrix Health's Medical Revenue Service (Case Study)
| Category | In-House Billing | With Veltrix Health | Results |
|---|---|---|---|
| Charges (on average) | $142,000.00 | $142,000.00 | N/A |
| Gross Collection Rate (GCR) | $60,000 (42%) | $77,000 (54%) | 12% Increase in Gross Collection Rate |
| Billing Costs | $6,000 | $4,000 | $2,000 Decrease in monthly cost of RCM service |
End-to-End RCM Service Features by Veltrix Health
You have nothing to lose, and everything to gain with Urgent RCM Medical Revenue Cycle Management features. This means our healthcare RCM service is the partner you can trust for your revenue cycle success.
Veltrix Service Features
These features ensure your revenue cycle is optimized for success, with Urgent RCM handling every step for you.
Charge Entry Feature
- Claim creation, validation, and transmission
- Entering valid superbill information
- Claim approval confirmation
- Claim status tracking
Remittance Processing Feature
- Processing of payments from the payers
- Processing of adjustments and denials
- Reconciling payments to the provider's claims
Insurance Follow-Up Feature
- Following up with payers for unpaid claims
- Following up with payers for underpaid claims
- Contact payers on a provider's behalf
- Negotiating and resolving claim disputes
KPI Reporting & Analytics
- Monitors your key performance indicators
- Analyzes days in accounts receivable
- Analyzes claim denial rate and collection rate
- Comprehensive and customizable reports
- Advanced data visualization tools
Patient Collections Feature
- Collecting patient payments
- Managing initial statement + final notice
- Sending clean bills and reminders to patients
- Convenient payment options for patients
A/R Management Feature
- A/R workflow optimization
- Claim approval confirmation
- Collecting A/R collections from the payers and patients
Coding and Documentation
- Coding provider's services compliantly
- Using the latest coding standards and guidelines
- Capturing relevant details that support a provider's claims
- Justifying a provider's reimbursement for their services
- Performing medical bill audits
Contract Management
- Managing contractual agreements with the payers
- Determining how much you get paid for your services
- Reviewing and negotiating your contracts
- Monitoring the contracts' compliance
- Analyzing the contract performance
- Using metrics like contract yield and case mix index (CMI)
Resolving Healthcare Providers' Challenges
Poor Cash Flow
Healthcare providers struggle to maintain a consistent and predictable income due to unpaid bills and lower-than-expected payments.
Better Cash Flow
Our medical revenue cycle management (RCM) service reduces lousy debt and underpayments by ensuring accurate and timely claim submission and follow-up.
Mishandled A/R
Providers encounter challenges managing their accounts receivable (A/R) due to the complex and variable nature of the process.
Managed A/R
Our healthcare revenue cycle management (RCM) solution offers insight into A/R performance, including days in A/R, A/R aging, and A/R turnover.
Misaligned Payer Compatibility
Providers face challenges in meeting the requirements of multiple payers and various claim types, such as fee-for-service, value-based, and capitated.
Aligned Payer Compatibility
Our adaptable and expandable RCM platform adjusts to evolving payer requirements and optimizes provider reimbursements.
High Denial Rates
Providers experience a high rate of payer denials, which negatively impacts their revenue and cash flow.
High Recovery Rates
Our proactive and preventive approach resolves the root causes of denials to enhance denial recovery rates and revenue integrity.
More Admin Workload
Denials result in reduced provider revenue collection and increased workload due to the need to appeal and resubmit claims.
Automated Process
Our RCM experts and EHR platform automate manual work and ensure accurate claim submissions.
Unsatisfied Patients
Providers are struggling to ensure patient satisfaction as patients increasingly take control of their healthcare decisions.
Satisfied Patients
Our revenue cycle management (RCM) service provides a patient-centric platform with telehealth features to enhance the patient-payer relationship.
Complicated Patient Management
Providers are facing challenges coping with the growing financial responsibility of patients, attributed to high deductible health plans (HDHPs) and self-pay individuals.
Automated Patient Management
Our medical billing platform automatically estimates and communicates the patient's out-of-pocket costs before the service.
REPORTING & ANALYTICS FEATURES
Choose Veltrix Health Billing Company For Complete Revenue Cycle Management Reporting

Data Insights
Check out the primary data and trends of the revenue billing process in a detailed and interactive analytics dashboard. You can compare how you're doing with industry standards and find areas to improve.
Quick Feedback
Use our integrated chat system to instantly talk to our experts, your patients, and the insurance payers. You can ask questions, share feedback, and solve problems in real-time.
Detailed Reports
Quickly analyze your revenue cycle using our customizable and detailed reports. You can organize, arrange, and download medical billing data based on your specific requirements and preferences.

Multi-Specialty Support
Manage multiple facilities and locations with our RCM reporting dashboard. You can view and compare data from different sites and groups in one place—a dedicated dashboard for each specialty.
Data Security
You can trust that we keep your data safe and secure. We use the newest encryption and authentication technologies to prevent unauthorized access and breaches of your data.
Data Integration
At Veltrix Health, our RCM reporting dashboard makes it easy to connect your data with other systems and platforms. We support various formats and standards to ensure smooth data exchange and compatibility.
Frequently Asked Questions

Revenue Cycle Services can enhance medical revenue by improving coding accuracy, reducing claim denials, optimizing billing processes, and ensuring timely reimbursement. These services focus on maximizing revenue potential for healthcare providers.
Revenue Cycle Optimization offers several benefits, including improved cash flow, reduced billing errors, enhanced operational efficiency, minimized revenue leakage, better compliance, and increased overall profitability for healthcare organizations.
Urgent RCM addresses credit balance issues through rigorous auditing, proactive reconciliation processes, and advanced reporting tools. By identifying and resolving credit balance discrepancies promptly, we help healthcare providers maintain financial integrity.
End-to-End Revenue Cycle Management services include patient access solutions (such as scheduling and eligibility verification), clinical documentation and coding, revenue cycle operations (like accounts receivable management and denial management), and patient financial services.